Estimated reading time: 9 minute(s)
The IRS is following patterns from previous reporting years, as they have offered up some relief when it comes to ACA reporting. Before you get too excited, most of the reporting requirements are unaffected and must be carried out as expected in order to avoid any IRS penalties.
This is what mandated reporters need to know going into 2021.
The Recipient Copy Deadline
As you may have heard, the IRS has extended the deadline to distribute recipient copies from January 31, 2021 to March 2, 2021.
This deadline extension shouldn’t be confused with the deadline to file Forms 1094 and 1095 with the IRS, these deadlines will not be affected. Paper forms must be submitted to the IRS on March 1, 2021, or filed electronically by March 31, 2021.
Click here to learn more about the State filing deadlines.
Relief Regarding Form 1095-B
Now that the individual mandate is no longer in place, the need for certain information returns being furnished to recipients is a less pressing matter. For example, when it comes to Form 1095-B, the IRS is not penalizing organizations for the failure of providing recipient copies under two conditions. First, the employer must make it abundantly clear on its website that the 1095-B is available upon request. Second, for the individuals that do make this request, the recipient copy must be supplied within 30 days. Both of these conditions must be met.
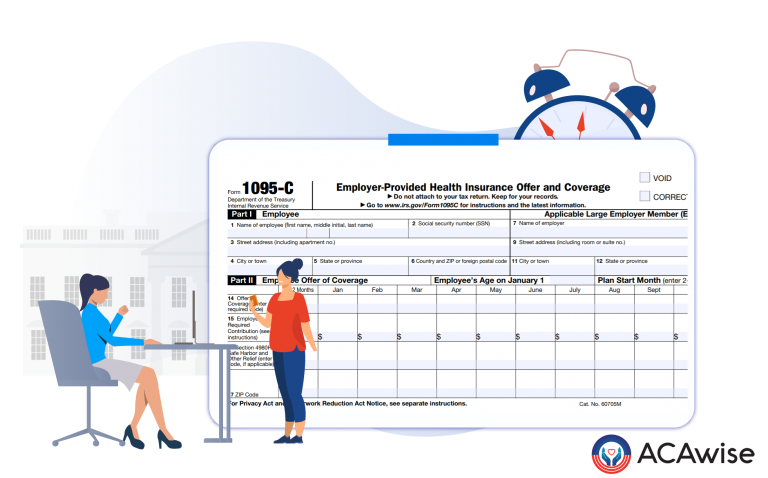
Relief Regarding Form 1095-C
As for Form 1095-C, the IRS will not impose a penalty for failure to furnish it to any employee enrolled in an ALE member’s self-insured health plan who is not a full-time employee for any month of 2020. Employers must meet this condition by completing Part 1 of the Form 1095-C and indicating Code 1G for this employee in the IRS reporting. See Notice 2020-76 for more information on reporting penalties.
Remember, The 2020 section 6055 furnishing relief in no way affects the assessment of penalties associated with the requirement or the deadline to file with the IRS the 2020 Forms 1094-B or 1095-B or the Forms 1094-C or 1095-C, as applicable.
Relief for Inaccuracies in Reporting
There is a little more good news when it comes to IRS penalties for ACA reporting. When it comes to inaccuracies and missing information, the IRS is willing to cut filers some slack. When it comes to an incorrect TIN/SSN or an inaccurate date of birth, the IRS is willing to overlook penalizing these errors. Provided that the filer acted in good faith and indeed took the necessary steps to complete their ACA reporting to the best of their ability.
This nicety does NOT extend to mandated filers that fail to file their ACA reporting entirely and make no effort to distribute their recipient copies to their employees.
There’s no need to worry about penalties for your 2021 ACA reporting! ACAwise is here to help! We are prepared with the latest updates from the IRS and our team of experts can help you create a game plan for your on-time and accurate reporting this year.
Incorrect TINs? Missing information? There’s no need for that, with ACAwise, we run your information through data validations to ensure accuracy. We even completely generate your ACA codes!
Learn more about the ACAwise services today!

Leave a Comment